Florida Blue Provider Appeal Form - Forms for florida blue members enrolled in individual, family and employer plans. These requests are referred to as appeals. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. Help your florida blue patients understand their. Physicians and providers may request reconsideration of how a claim processed, paid or denied. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. Find commonly used physician, provider and member forms for you to complete and send to us. The most commonly used physician and provider forms are.
When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. Help your florida blue patients understand their. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. Forms for florida blue members enrolled in individual, family and employer plans. These requests are referred to as appeals. The most commonly used physician and provider forms are. Find commonly used physician, provider and member forms for you to complete and send to us. Physicians and providers may request reconsideration of how a claim processed, paid or denied.
Help your florida blue patients understand their. Forms for florida blue members enrolled in individual, family and employer plans. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. The most commonly used physician and provider forms are. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. Find commonly used physician, provider and member forms for you to complete and send to us. These requests are referred to as appeals. Physicians and providers may request reconsideration of how a claim processed, paid or denied.
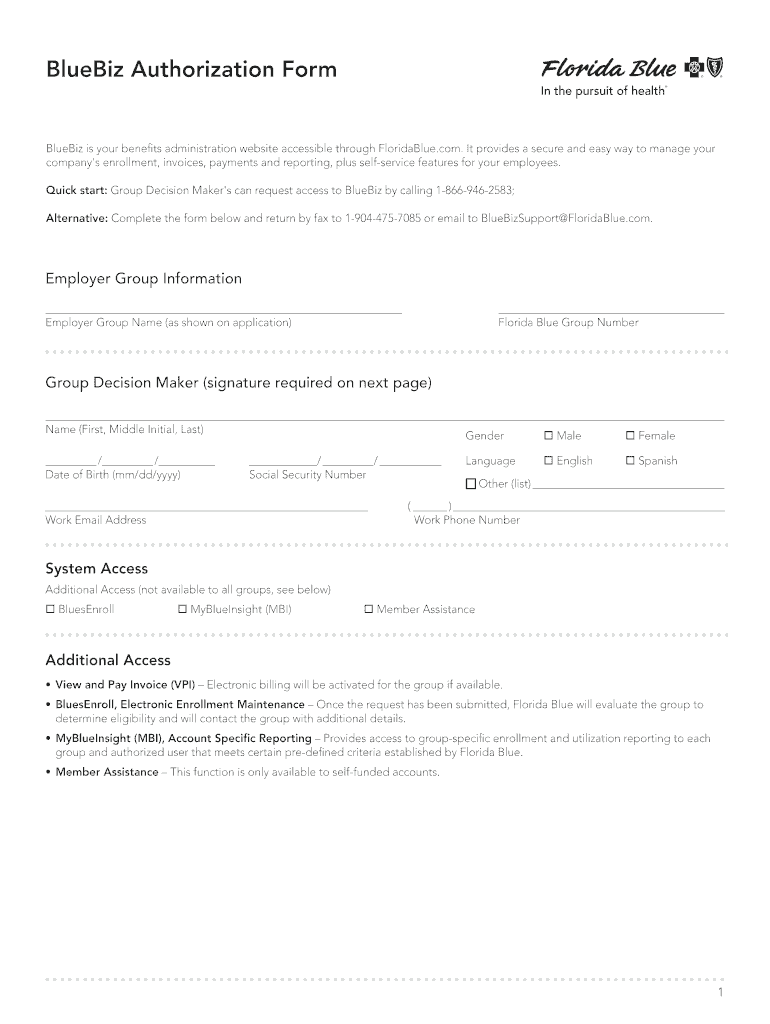
Fl Blue Authorization Form Fill Online, Printable, Fillable
These requests are referred to as appeals. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. The most commonly used physician and provider forms are. Find commonly used physician, provider and member forms for you to complete and send to us. Help your florida blue patients understand their.
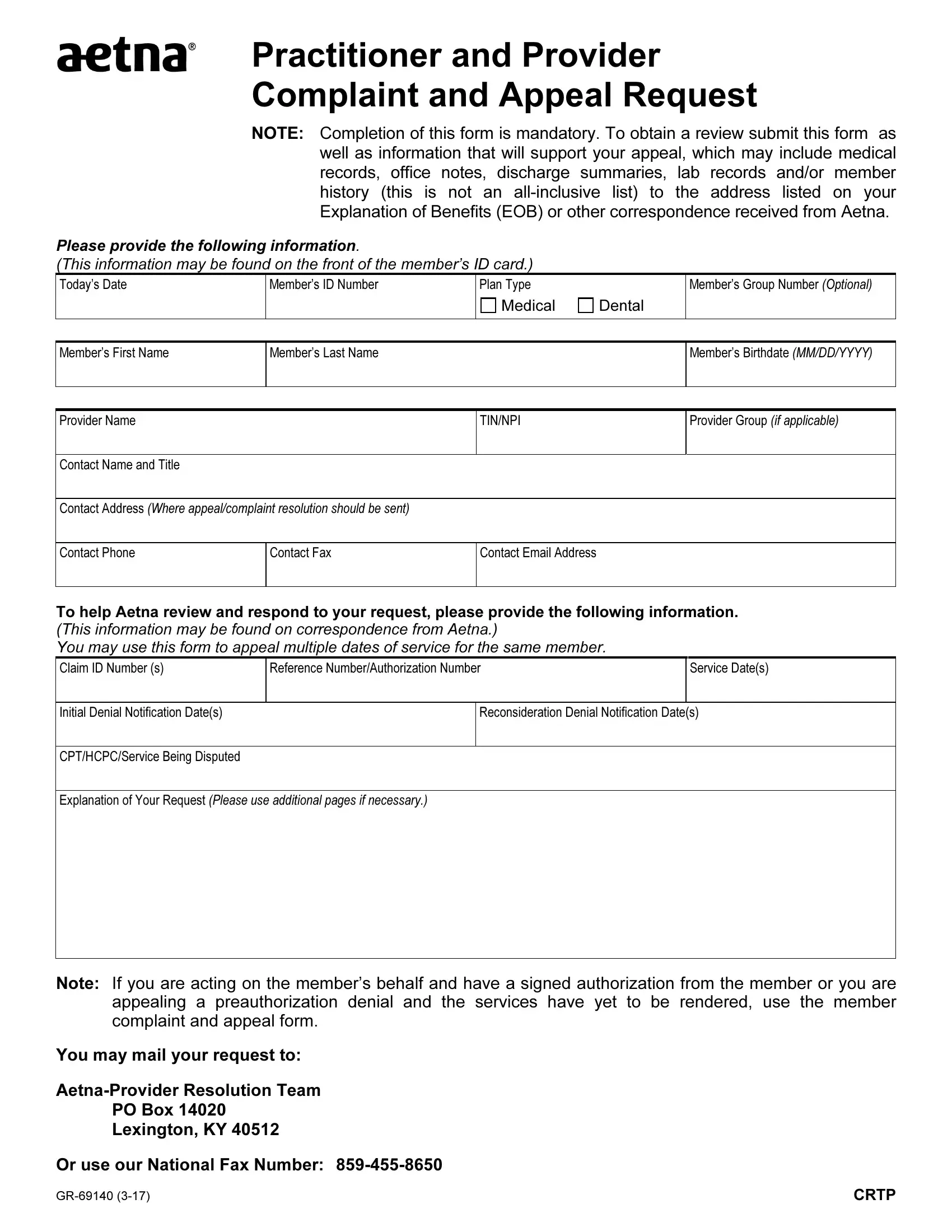
Aetna Appeal Form ≡ Fill Out Printable PDF Forms Online
Forms for florida blue members enrolled in individual, family and employer plans. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. The most commonly used physician and provider forms are. Find commonly used physician, provider and member forms for you to complete and send to us..
Provider Information Update Form Provider Manual Florida Blue
Physicians and providers may request reconsideration of how a claim processed, paid or denied. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. The most commonly.
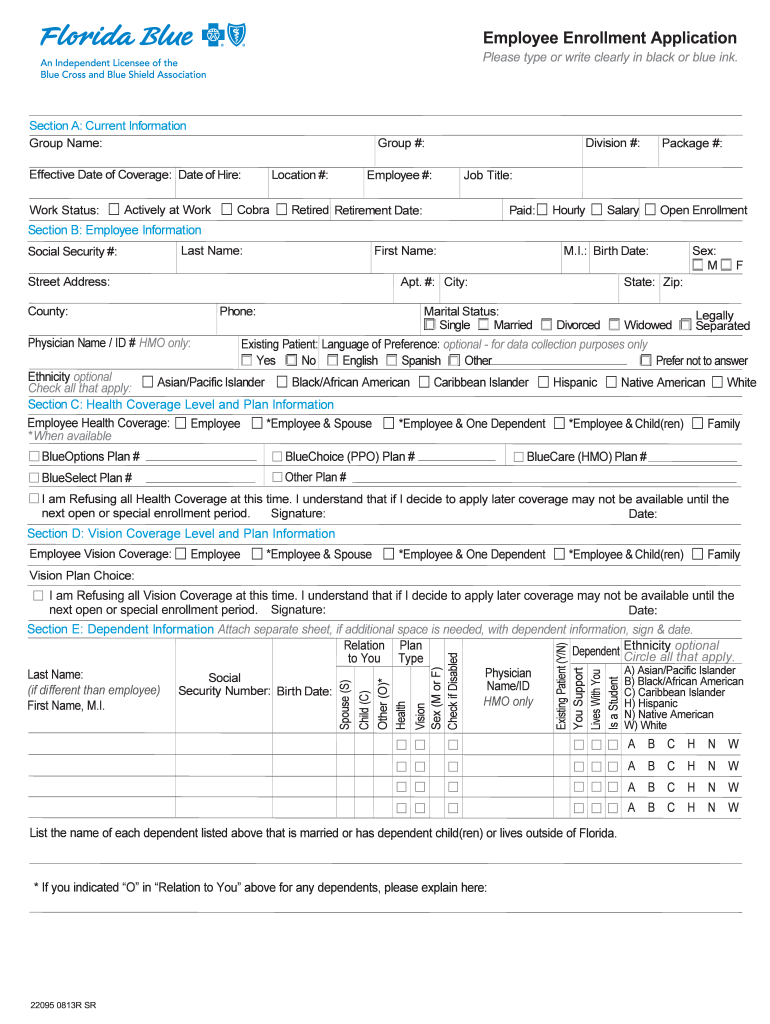
Bcbsfl Fill out & sign online DocHub
When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. These requests are referred to as appeals. Physicians and providers may request reconsideration of how a claim processed, paid or denied. Forms for florida blue members enrolled in individual, family and employer plans. The most commonly used.
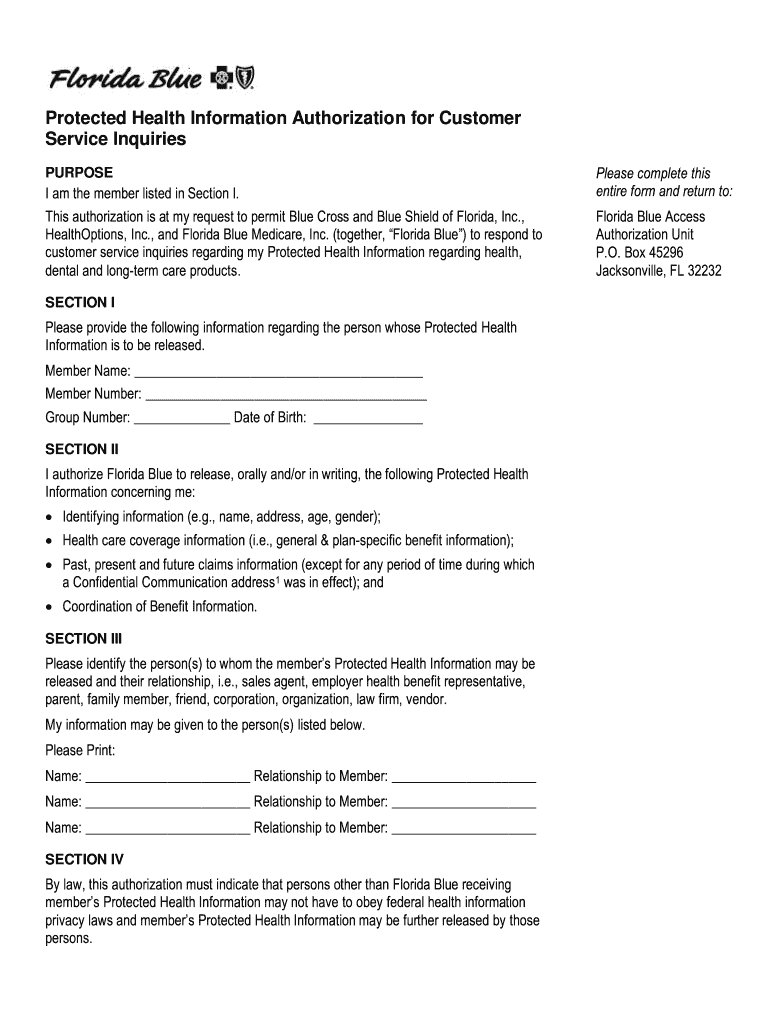
Florida Blue Y0011_30871 2019 Fill and Sign Printable Template Online
To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. Help your florida blue patients understand their. Forms for florida blue members enrolled in individual, family and employer plans. Find commonly used physician, provider and member forms for you to complete and send to us. These requests are referred to.
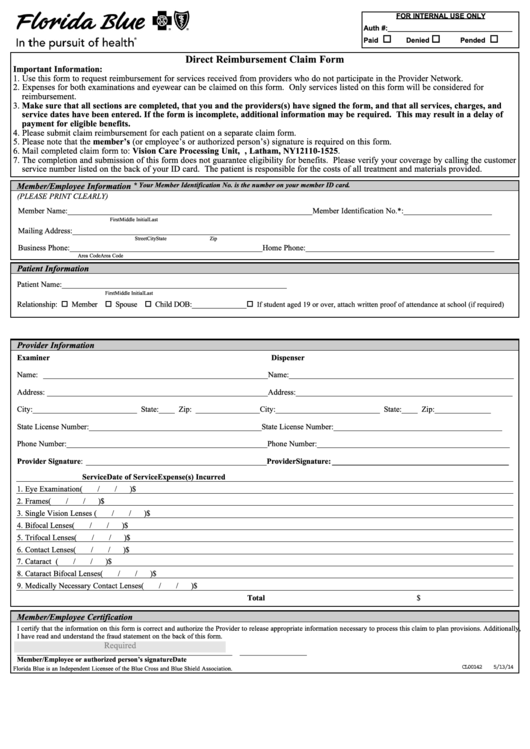
Direct Reimbursement Claim Form Florida Blue printable pdf download
Forms for florida blue members enrolled in individual, family and employer plans. Help your florida blue patients understand their. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your.
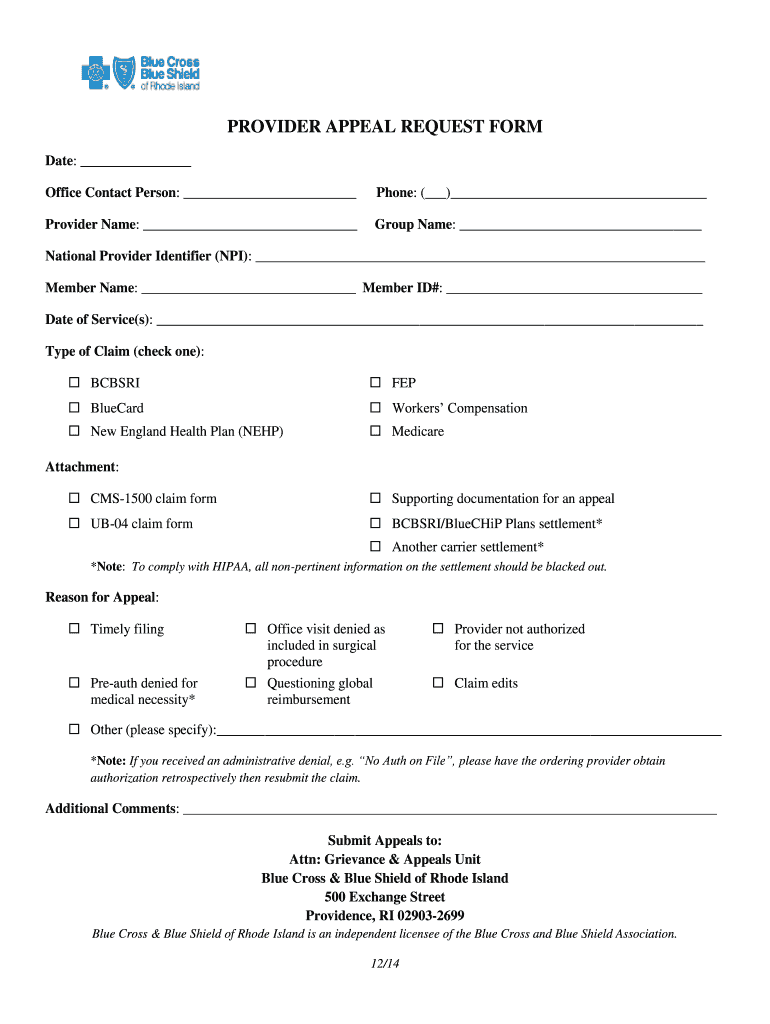
Fillable Online PROVIDER APPEAL REQUEST FORM Fax Email Print pdfFiller
These requests are referred to as appeals. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. Help your florida blue patients understand their. Forms for florida blue members enrolled in individual, family and employer plans. The most commonly used physician and provider forms are.
Anthem provider appeal form pdf Fill out & sign online DocHub
Help your florida blue patients understand their. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. The most commonly used physician and provider forms are. Forms for florida blue members enrolled in individual, family and employer plans. Physicians and providers may request reconsideration of how a.
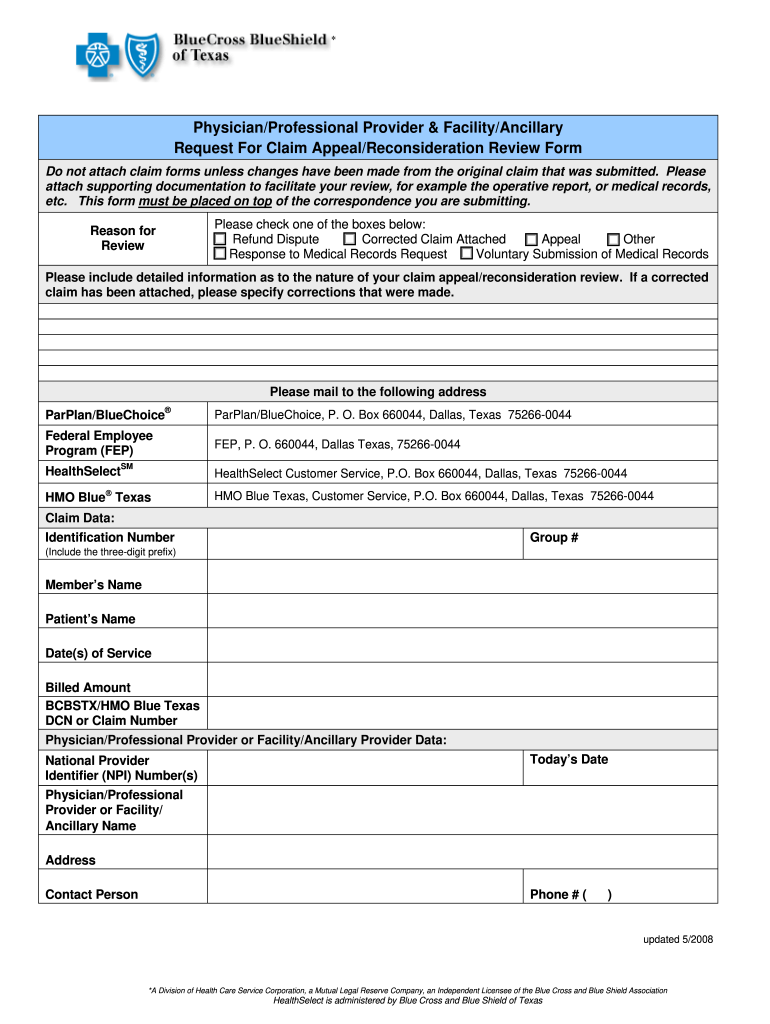
Bcbs Request Claim 20082025 Form Fill Out and Sign Printable PDF
Forms for florida blue members enrolled in individual, family and employer plans. Help your florida blue patients understand their. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s manual for. The most commonly used physician and provider forms are. Physicians and providers may request reconsideration of how a.
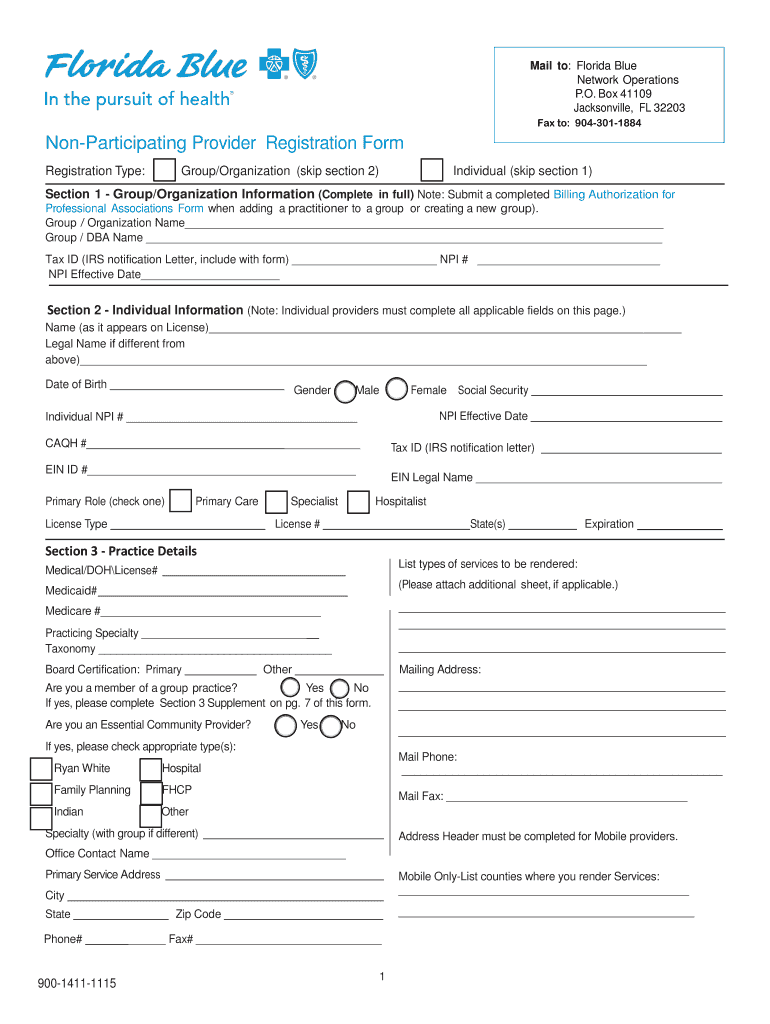
Florida Blue Non Participating Provider Form Fill Online, Printable
The most commonly used physician and provider forms are. These requests are referred to as appeals. Help your florida blue patients understand their. Find commonly used physician, provider and member forms for you to complete and send to us. When submitting a provider appeal, please complete the form in its entirety in accordance with the instructions contained in florida blue’s.
Forms For Florida Blue Members Enrolled In Individual, Family And Employer Plans.
Help your florida blue patients understand their. The most commonly used physician and provider forms are. To ensure value from your plan benefits it is important that your physician obtains prior authorization for your medical services. These requests are referred to as appeals.
When Submitting A Provider Appeal, Please Complete The Form In Its Entirety In Accordance With The Instructions Contained In Florida Blue’s Manual For.
Physicians and providers may request reconsideration of how a claim processed, paid or denied. Find commonly used physician, provider and member forms for you to complete and send to us.